Part 2: Understanding the Knee Joint: Why It Breaks Down (and Why Surgery Can’t Fully Replace It)
Jun 27, 2025

We tend to think of joints like car parts—wear them down, swap them out, good as new, right? But your knee is not a bolt-on piece of equipment. It’s a living, moving, deeply complex structure, and once it starts to break down, replacing it is never as simple—or as perfect—as people are led to believe.
Let’s break down what makes the knee so special… and why even the most advanced surgical replacements can’t quite measure up to what nature gave us.
First, a Quick (Fun) Anatomy Lesson—No Heavy Jargon, Promise
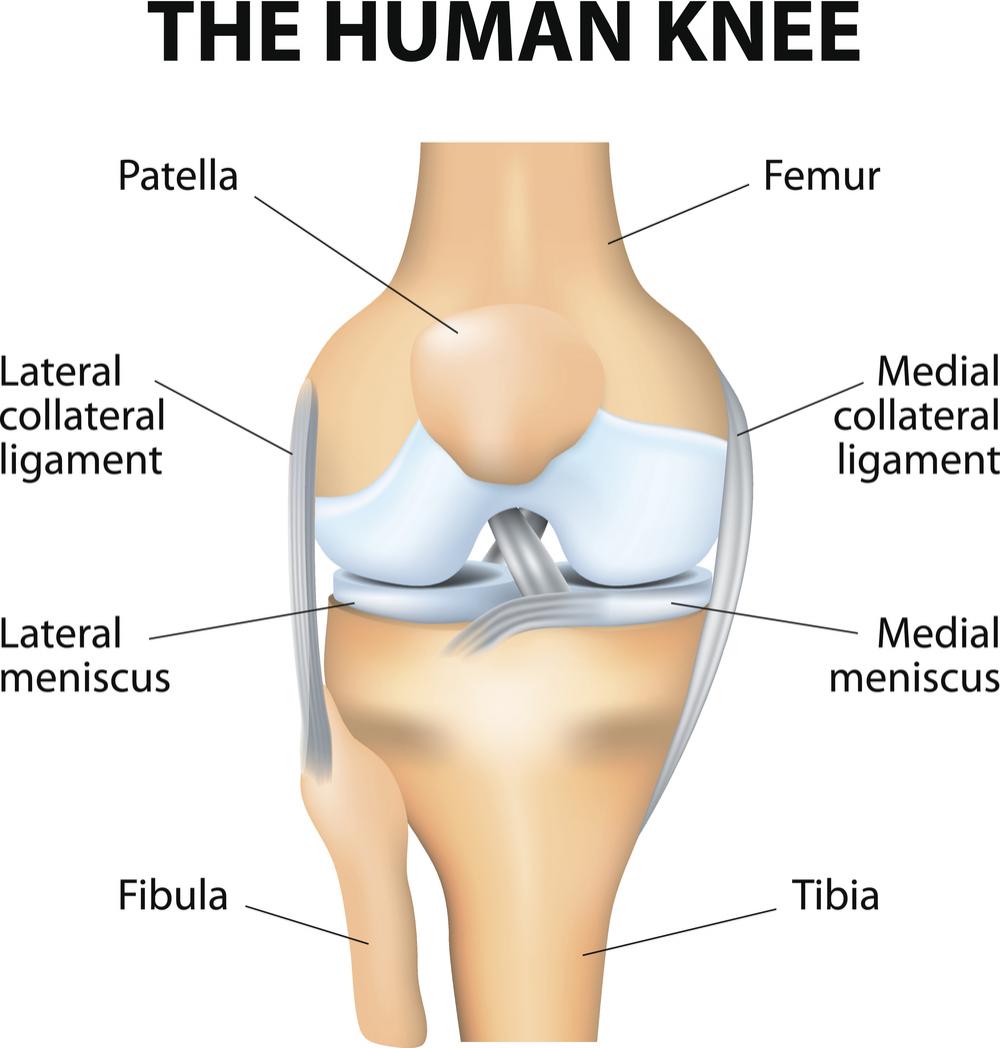
Your knee isn’t just a hinge. It’s a brilliant little engineering marvel made up of three bones: the femur (thigh), tibia (shin), and patella (kneecap). Between them are layers of cartilage, ligaments that stabilize motion, and soft tissue that guides smooth, shock-absorbed movement.
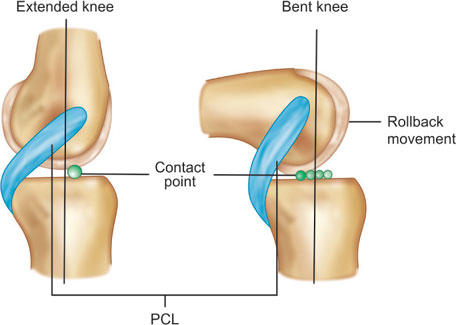
But here’s where it gets juicy: the femur’s condyles—those rounded ends that sit on top of the tibia—aren’t symmetrical. The medial (inner) side is larger and shaped differently than the lateral (outer) side. Why? Because your knee doesn’t just bend and straighten. It rolls, glides, and rotates—especially in deep flexion, like squatting, kneeling, or sitting cross-legged. The asymmetry is what allows for that natural “roll-back” as your knee bends.
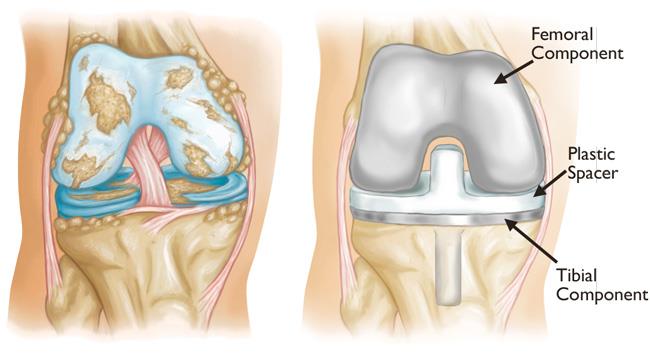
So… What Happens When You Replace a Knee?
When a surgeon performs a total knee replacement, they cut away the natural condyles of your femur and replace them with metal implants—and here’s the catch: most hardware is designed symmetrically. That’s right. They take a joint designed for asymmetrical motion and install something that’s geometrically balanced.
The result? You lose the natural roll-back. Deep flexion becomes harder, sometimes impossible. Movements like kneeling or squatting may feel awkward, restricted, or even painful. And while many people are told, “You’ll be back to normal in no time!”—the reality is, your biomechanics are permanently changed.
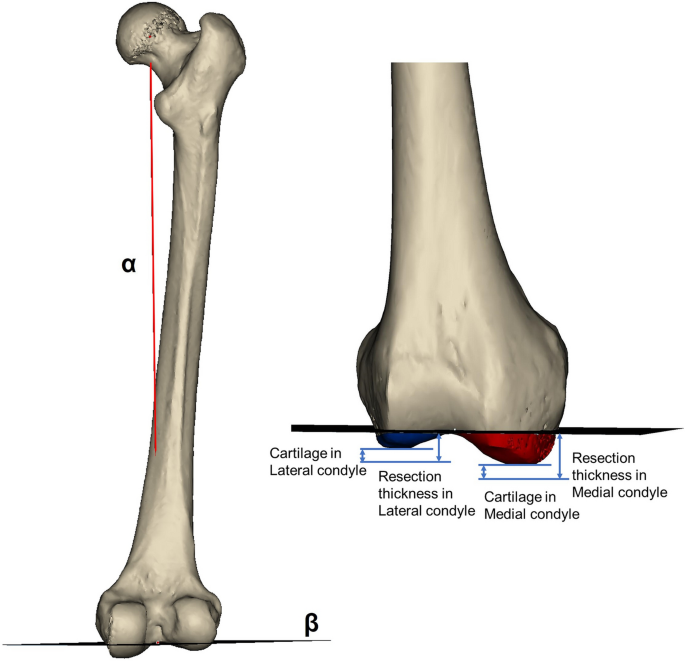
Medial Wear: The Silent Creep Toward Surgery
Remember how we said the inner condyle is larger? That means it takes on more load, especially when your movement patterns are off—like when your glutes are weak, you walk with poor alignment, or you've had years of inflammation eating away at the joint. This leads to asymmetrical wear, which is why so many people end up with that classic “bone-on-bone on the inside” diagnosis.
But here’s the thing: wear doesn’t happen in a vacuum. It’s not just “old age” or “bad luck.” It’s movement, inflammation, muscle balance, and repetitive stress. Which means there’s often a window to correct the course—before things spiral into surgery.
Why You May Never Feel "Normal" After a Replacement
Even with perfect surgical technique and the latest prosthetic, the truth is: you’re never getting your original joint back. And it’s not just about range of motion—it’s about the feel. People often report stiffness, odd sensations, clunking sounds, or a general sense that the knee just doesn’t “belong” to them anymore.
And that makes sense. Your natural joint could subtly rotate, adjust, and adapt with each step. A prosthetic knee? Not so much. It’s fixed, it’s mechanical, and it’s limited.
So yes, it can relieve severe pain, and in many cases, it improves basic function—but we need to stop selling the idea that it’s a complete “restoration.” It’s more like a hardware patch job. And for some, that’s fine! But for others—especially younger or more active folks—it can be incredibly frustrating.
What This Means for Prevention
Understanding the real mechanics of your knee should inspire proactive care. If we want to avoid the limitations of a prosthetic knee, we need to:
-
Preserve cartilage and joint space through anti-inflammatory nutrition
-
Strengthen glutes, quads, and core to balance knee load
-
Improve mobility in the hips and ankles (because the knee suffers when they don’t move well)
-
Use acupuncture and soft tissue therapy to reduce pain and inflammation early—not after years of breakdown
Because the best knee replacement is… not needing one.
Coming Up Next...
In Part 3, I’ll take you into the operating room—what actually happens during a total knee replacement, what gets removed, what goes in, and the reality behind recovery timelines.
For now, I hope this helps you see your knees not just as joints—but as intelligent, dynamic systems worth preserving.
If you’re feeling pain, stiffness, or confusion about what to do next—remember, there’s help. And there’s time.
Let’s make decisions that honor your body’s brilliance.
Keep moving, eat something green, and question anything that sounds like a quick fix.
Chow! Chow!