Part 4: Questions to Ask Before You Say Yes to Knee Replacement Surgery
Jul 11, 2025

Let’s set the scene: you’ve been in pain for a while. You’ve tried some over-the-counter meds, maybe a few doctor visits, and possibly had a local injection or two. At some point, someone mentions “bone-on-bone,” and just like that, you’re booked for a knee replacement in two weeks. Quick consult. Big decision. Minimal information.
But I’m here to hit pause.
As someone who’s worked on both sides of the surgical curtain—first as an orthopedic sales rep in the OR, and now as a practitioner focused on structural integration, movement, and acupuncture—I can tell you: this decision deserves more. More clarity. More context. More you in the driver’s seat.
So let’s talk about the questions you should ask, the assumptions to challenge, and the ways to reclaim your power before you let anyone wheel you toward the OR.
“Have I Truly Addressed the Root Cause?”
This is the question no one can answer but you—and it requires honesty.
Have you:
-
Worked on how you stand, walk, and move?
-
Explored postural therapy or structural integration (like Rolfing)?
-
Committed to gait retraining and muscle activation patterns?
-
Cleaned up your diet and lifestyle to reduce systemic inflammation?
-
Gotten support to address stress, sleep, and movement habits?
Or have you been sold a series of quick fixes—NSAIDs, gabapentin, a few physical therapy sessions, maybe even a corticosteroid injection—without ever being told what’s really happening in your body?
Because here’s the hard truth: cortisone is not a solution.
It doesn’t “fix” anything. It kills off the nerves in the area to mute the pain signal. That’s why patients are typically only allowed a maximum of three injections in one area—it causes irreversible nerve damage and deteriorates surrounding tissues.
What most people aren’t told is this:
-
When nerves are killed, the brain can’t signal that something’s wrong anymore. Pain may go down, but injury risk goes up because the body’s feedback loop is offline.
-
The nerves do grow back—but not in the same pattern. That’s why a second or third injection often doesn’t “work.” There are no longer any nerves in that exact spot to silence.
-
And all the while, the true root cause—how you move, load, and live—is being ignored. Or worse, allowed to worsen in silence.
“Am I Relying on Passive Solutions—or Am I Rebuilding My Body?”
There’s a world of difference between supporting your body and outsourcing your health.
Braces, orthotics, and injections may feel helpful in the short term—but they rarely change the trajectory. What I recommend instead:
-
Gait retraining to teach your body to move with better mechanics
-
Postural therapy to realign joints and relieve compensatory strain
-
Structural integration (like Rolfing) to reset muscle memory and fascial holding patterns
-
Consistent, functional strength work focused on the glutes, hips, core, and feet
Yes, these require work. They require you. But they also build strength, awareness, and long-term resilience.
And here’s where I want to speak directly from the heart:
Taking responsibility for your pain is hard—especially if the root cause is your lifestyle, movement habits, or how you treat your body. That’s a tough mirror to stand in front of. But it’s also the most liberating realization you’ll ever have.
Because if you are the problem...
Then you are also the solution.
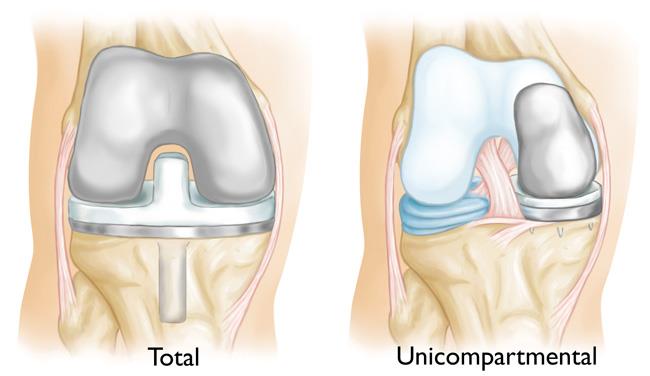
“Do I Even Need a Total Replacement?”
Not all arthritis is created equal. Sometimes, only part of the knee is damaged—especially the medial (inner) compartment. Yet many people are rushed into a full knee replacement when they might qualify for a partial (unicompartmental) replacement, which is less invasive, preserves more of the natural joint, and often feels more “normal” post-op.
Ask:
🗣️ “Is a partial knee replacement an option for me? And if not, why?”
Just know that not every surgeon offers partials. If you get a vague or dismissive answer, it’s okay to seek a second opinion.
“What Implant Are You Using—And Is It Designed for Real Movement?”
This question could change everything.
Most implants are symmetrical, despite the fact that your natural femur isn’t. This symmetry limits natural roll-back and deep flexion, which means squatting, kneeling, and sitting cross-legged may never feel the same again.
Some companies—like Smith & Nephew, who I worked with—make more ergonomic designs (like the Journey II BCS) that mimic natural asymmetry and allow for more normal motion. But unless you ask, you may never know what implant you’re getting.
Ask:
🗣️ “What brand and model implant are you using, and why?”
🗣️ “Does it support roll-back and high flexion?”
This is your body. You have every right to know what’s going inside it.
“What Happens If I Wait?”
You don’t have to rush.
Unless you’re facing severe instability, bone collapse, or joint infection, most people can safely delay surgery—especially if they use that time to improve strength, reduce inflammation, and work on movement patterns.
And here's something many people discover:
When you start addressing how you move, what you eat, and how you live, your pain often decreases… sometimes enough to delay surgery for years, or avoid it altogether.
So ask:
🗣️ “Would waiting 6–12 months while I focus on strength, nutrition, and functional movement worsen my condition—or potentially improve it?”
If your surgeon gives you pushback on that question, take note. And if they act offended or dismissive, consider it a red flag.
We are no longer in the age where a white coat equals unquestioned authority. The era of doctors as infallible gods is over—and good riddance. Patients today are informed, empowered, and surrounded by clinical research that clearly shows the impact of lifestyle, diet, and movement—especially for people with surgical hardware.
A truly good surgeon will respect your curiosity and welcome a conversation. If yours doesn’t, find one who does.

“What Happens If It Doesn’t Work?”
No one wants to think about failed outcomes—but they happen. Some people still have pain. Some develop stiffness or regret. Some need a revision within 5–10 years.
Ask your surgeon:
-
“What’s your revision rate?”
-
“What percentage of your patients still have symptoms after surgery?”
-
“What are my options if I’m not satisfied with the result?”
Transparency matters. And you should never be gaslit or dismissed for asking real questions about your body and your future.
Create a Palace, Not a Cage
You weren’t born broken. You weren’t meant to live in pain. But if you’ve ignored your body for years, fed it junk, and moved it poorly… it’s going to speak up. Loudly.
And yes, that’s hard to face. But it’s also an invitation to transform.
“Nothing in life matters—not the food, the car, or the cash—if you don’t have your health and can’t feel at home in your body.”
Your body can be a palace—strong, mobile, pain-free, and expansive. Or it can be a cage, stiff, inflamed, and full of restriction. The difference? Your choices. Your ownership. Your willingness to do the work.

In Part 5, we’ll dive into life after knee replacement—what recovery is really like, what people wish they’d known, and how to get the most from your new joint if surgery truly was your best move.
Until then…
Keep moving, eat something green, and question anything that sounds like a quick fix.
Chow! Chow!
Note: Mention of Smith & Nephew reflects my personal experience in the OR and is not a paid promotion or endorsement. I do not align with or promote any specific orthopedic brand.