Why Are Your Fingers Going Numb at Night?
numbness pain management postural awareness shoulder pain sleep Apr 17, 2024Do you ever wake up in the middle of the night with your fingers feeling numb and tingly? It's a common complaint that can disrupt your sleep and leave you feeling puzzled about its cause. However, there's a fascinating connection between the anatomy of your cervical vertebrae (neck) and your shoulder that might hold the key to understanding this discomfort.

The Anatomy Link: Cervical Vertebrae and Shoulder
The cervical vertebrae consist of seven small bones stacked on top of each other in the neck region. These vertebrae provide support for the head and neck while allowing for a wide range of motion, including flexion, extension, rotation, and lateral bending.
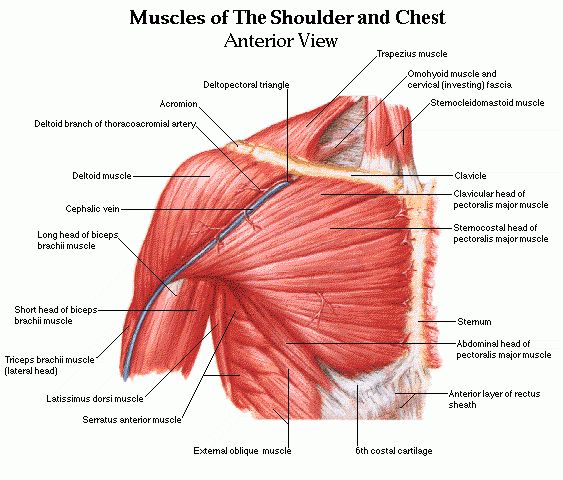
Surrounding the cervical vertebrae are layers of muscles and soft tissues that play a vital role in stabilizing the neck and supporting its movements. Some of the key muscles and soft tissues involved include:
-
Trapezius: This large muscle extends from the base of the skull down to the middle of the back and across the shoulders. It helps to stabilize and move the shoulder blades and plays a role in neck movement.
-
Levator Scapulae: Situated along the side and back of the neck, this muscle elevates the shoulder blades and assists in neck movement.
-
Rhomboids: Located between the shoulder blades, the rhomboid muscles retract the shoulder blades, helping to maintain proper posture and shoulder alignment.
-
Sternocleidomastoid: This muscle runs along the side of the neck and connects to the sternum and clavicle. It allows for rotation and flexion of the head and neck.
-
Deltoid: The deltoid muscle covers the shoulder joint and is responsible for various shoulder movements, including abduction, flexion, and extension.
These muscles and soft tissues work together to provide stability and mobility to the upper body, facilitating movements of the head, neck, and shoulders.
Brachial Plexus and Arm Control:
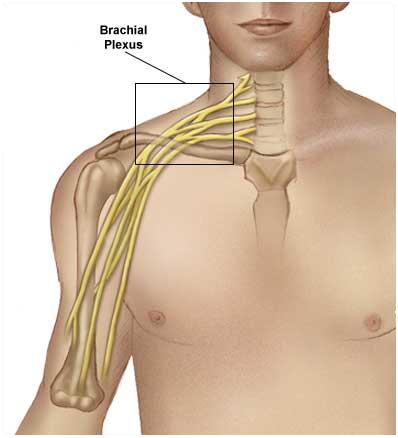
The brachial plexus is a network of nerves that originates from the spinal cord in the neck (specifically the cervical spine) and extends into the shoulder and upper arm. It is formed by the anterior rami of the lower four cervical nerves (C5-C8) and the first thoracic nerve (T1).
The brachial plexus is responsible for providing sensory and motor innervation to the muscles and skin of the shoulder, arm, and hand. It controls movement and sensation in these areas, allowing us to perform various tasks with our arms, such as reaching, grasping, and lifting.
When the muscles and soft tissues surrounding the cervical vertebrae and shoulder become tight or inflamed, they can compress the nerves of the brachial plexus, leading to symptoms such as pain, numbness, tingling, and weakness in the arm and hand. This compression can occur due to poor posture, repetitive movements, injury, or underlying medical conditions.
Therefore, maintaining optimal posture, flexibility, and strength in the muscles surrounding the cervical spine and shoulder is crucial for preventing compression of the brachial plexus and ensuring proper arm function.
In summary, the anatomy of the cervical vertebrae, shoulder, and brachial plexus are intricately linked, with muscles and soft tissues connecting them and working together to support and move the upper body. Understanding this interconnectedness can help in identifying and addressing issues related to neck and shoulder discomfort, as well as maintaining optimal arm function.
Distinguishing Between Brachial Plexus Impingement and Thoracic Outlet Syndrome
Anatomy and Mechanism:
Brachial plexus impingement and thoracic outlet syndrome (TOS) both involve compression of neurovascular structures in the upper body, leading to symptoms such as pain, numbness, tingling, and weakness in the shoulder, arm, and hand. However, they differ in their underlying anatomical locations and mechanisms of compression.
-
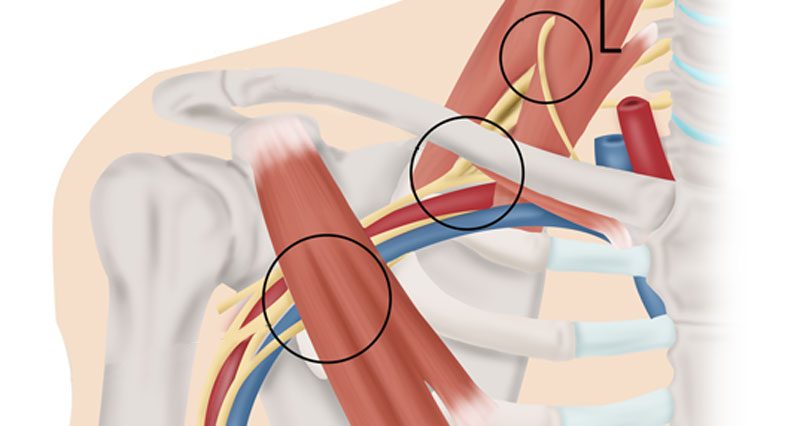
Brachial Plexus Impingement: This condition occurs when the nerves of the brachial plexus, originating from the cervical spine, become compressed or irritated. Factors such as poor posture, trauma, or repetitive motions can contribute to compression of the nerves as they exit the cervical spine. Muscle tightness, particularly in the scalene muscles of the neck, can exacerbate this compression, leading to symptoms along the distribution of the affected nerves.
-
Thoracic Outlet Syndrome: TOS involves compression of the neurovascular structures as they pass through the thoracic outlet—a narrow space between the collarbone (clavicle) and the first rib. This compression can affect the brachial plexus, as well as the subclavian artery and vein. TOS can result from various factors, including anatomical variations, muscle imbalances, trauma, or repetitive motions. Muscle tightness or hypertonicity, particularly in the scalene muscles and pectoralis minor, can contribute to compression of the neurovascular structures in the thoracic outlet.
Symptoms and Diagnostic:
While both conditions can cause similar symptoms in the shoulder, arm, and hand, their distribution and presentation may vary:
-
Brachial Plexus Impingement: Symptoms typically follow the distribution of the affected nerves, which can be mapped out using dermatomes. Pain, numbness, tingling, and weakness may be localized to specific dermatomes corresponding to the compressed nerves. For example, compression of the C5-C6 nerve roots may result in symptoms along the lateral aspect of the arm and into the thumb and index finger.
-
Thoracic Outlet Syndrome: Symptoms may be more diffuse and involve multiple dermatomes, depending on the extent of compression and the structures involved. Additionally, vascular symptoms such as arm pain, swelling, and discoloration, particularly with arm elevation, may be present in cases of vascular TOS.
Diagnosing brachial plexus impingement and thoracic outlet syndrome (TOS) typically involves a comprehensive evaluation by a healthcare professional, which may include:
- Clinical assessment: A thorough history and physical examination can help identify symptoms, assess muscle strength and sensation, and evaluate for signs of nerve or vascular compression.
- Imaging studies: X-rays, MRI, or CT scans may be used to assess the cervical spine, thoracic outlet, and surrounding structures for any anatomical abnormalities, such as bone spurs, herniated discs, or bony variations.
- Nerve conduction studies: Electromyography (EMG) and nerve conduction velocity (NCV) tests can help evaluate nerve function and identify areas of compression or damage.
- Provocative maneuvers: Specialized tests, such as Adson's test or Roos test, may be performed to reproduce symptoms and assess for thoracic outlet compression.

Management and Treatment:
-
Therapeutic Options for Relief:
- Physical Therapy: A tailored exercise program can help strengthen muscles, improve flexibility, and correct posture, reducing strain on the cervical spine and shoulders. Physical therapists may incorporate techniques such as nerve gliding exercises and myofascial release to alleviate compression.
- Chiropractic Care: Chiropractic adjustments may help realign the spine and reduce pressure on the nerves and blood vessels in the neck and shoulder region.
- Acupuncture: This traditional Chinese medicine practice involves the insertion of thin needles into specific points on the body to alleviate pain and promote healing. Many find relief from nerve-related symptoms through acupuncture.
- Massage Therapy: Targeted massage techniques can help release tension in muscles and soft tissues, improving circulation and reducing nerve compression.
-
Self-Care and Ergonomic Corrections:
- Postural Awareness: Practice mindful body awareness throughout the day, avoiding prolonged periods of slouching or forward head posture. Use cues such as setting reminders or adjusting workstation ergonomics to maintain proper alignment.
- Stretching and Strengthening Exercises: Incorporate regular stretching and strengthening exercises targeting the neck, shoulders, and upper back to improve muscle balance and posture.
- Ergonomic Adjustments: Make ergonomic adjustments to your workstation and daily activities, such as using supportive chairs, adjusting computer monitor height, and taking frequent breaks to stretch and move.
-
Posture While Sleeping:
- Use Supportive Pillows: Choose pillows that provide adequate support for your head, neck, and shoulders. Memory foam or contour pillows can help maintain proper alignment.
- Avoid Sleeping on Your Stomach: This position can strain the neck and exacerbate nerve compression. Instead, try sleeping on your back or side with a pillow between your knees for added support.
- Keep Your Spine Aligned: Ensure that your head, neck, and spine are in a neutral position while sleeping. Avoid propping multiple pillows under your head, as this can strain the neck.
Brachial plexus impingement and thoracic outlet syndrome can significantly impact daily functioning and quality of life. However, with proper diagnosis and a comprehensive management approach that includes conservative measures, self-care strategies, and ergonomic corrections, individuals can find relief from symptoms and improve their overall well-being. By prioritizing posture, incorporating therapeutic interventions, and making lifestyle adjustments, individuals can take proactive steps towards alleviating discomfort and optimizing their musculoskeletal health. If symptoms persist or worsen, it is essential to consult with a healthcare professional for further evaluation and guidance tailored to individual needs.
Other Considerations
- Ergonomic workspace: Maintain a proper ergonomic setup at your desk to prevent strain on the neck and shoulders during the day.
- Stress management: Stress can contribute to muscle tension and exacerbate symptoms. Incorporate relaxation techniques such as deep breathing, meditation, or yoga into your daily routine to help alleviate stress and tension.
In conclusion, the connection between the anatomy of the cervical vertebrae and shoulder sheds light on why you may experience numbness and tingling in your fingers at night. By understanding this link and implementing therapeutic strategies like physical therapy, chiropractic, acupuncture, and massage, along with practicing good posture both day and night, you can find relief and improve your overall well-being. If symptoms persist or worsen, be sure to consult with a healthcare professional for further evaluation and guidance.
Warm regards,
Jess
Categories